Pain care attracts a straight line between scientific research and mankind. Medical professionals bring that responsibility every shift, usually under time pressure and with incomplete details. A well created provide discomfort management program does greater than show medication graphes and pain ranges. It builds judgment, installs security practices, and offers clinicians the language to promote for people while securing themselves and their groups with strenuous documents and ethical practice.
I have actually instructed and refreshed pain management training across emergency divisions, rehab wards, and community setups. The themes listed below originated from genuine instances, debriefs after near misses out on, and lessons constructed right into standards such as PUAEME008 Supply Discomfort Monitoring in Australian prehospital contexts. Whether you are shaping pain administration training courses for registered nurses, physiotherapists, or mixed multidisciplinary associates, the exact same pillars persist: assessment, risk-free delivery, watchful tracking, clear documents, and ethical choice making.
What students require from a contemporary discomfort management course
When medical professionals sign up for short programs hurting monitoring, they often expect a formula: a dosage table for ketorolac, a titration system for fentanyl, a refresher on multimodal therapy. They do require those, yet they likewise need to practice the difficult parts that no flowchart will take care of. How to take care of an individual with extreme discomfort and a background of opioid use condition without preconception. When to stop escalating analgesia since the differential has actually altered. Exactly how to document acceleration and shared choices so the following medical professional can action in safely. Every solid pain management qualification training course ought to elevate these abilities together with pharmacology.
In emergency situation discomfort monitoring especially, very early decisions echo via a patient's journey. One ignored red flag or one undocumented adverse result can establish the phase for injury a number of hours later on. Courses that practice those inflection factors making use of instance vignettes and timed circumstances generate far better practices than lecture alone.
Safety as a skill, not a checklist
Safety suffering monitoring starts with identifying that analgesia is restorative and analysis. A dosage of IV morphine that fails to damage pain in a thought renal colic instance may change you towards a vascular or medical cause. Alternatively, quick relief after a sublingual GTN spray in upper body discomfort can misinform if you have not considered esophageal convulsion. Discomfort relief need to ride alongside a functioning diagnosis, not replace it.
I educate security along three tracks. First, pharmacologic safety: best client, best medicine, ideal dose, ideal route, right time. Second, physiologic safety and security: anticipate respiratory system clinical depression, hypotension, and transformed mental status, and have a strategy ready, not simply tools at the bedside. Third, system security: handover that carries the thread of what you attempted, what happened, and what you worried about.
Consider the frail older grown-up with a hip crack and standard eGFR in the 30s. A basic NSAID plan can worsen kidney feature. A single 5 mg oxycodone tablet might tip her into ecstasy. Excellent pain monitoring training for nurses and junior medical professionals imitates this compromise. You can still provide efficient analgesia, yet you might lean on local strategies, acetaminophen at scheduled intervals, and cautious opioid titration with frequent review. The program must also educate when to request for aid, for example, calling anesthetics for a fascia iliaca block instead of chasing after greater systemic doses.
The professional analysis that prevents errors
Before any individual grabs a syringe, they need a crisp, reproducible analysis. The lines in between neuropathic, nociceptive, and visceral pain matter since they forecast what jobs. A client explaining electrical shocks with allodynia along a dermatomal circulation will certainly not react well to rising pure mu agonists alone. Gabapentinoids, topical anesthetics, or a nerve block might provide relief with less risks.
An excellent supply pain administration course builds muscle memory around background and examination under various problems. In the rescue bay with sound and a time crunch, you may obtain a three inquiry pain history and a quick display for warnings, after that reassess after the first treatment. On a ward round, you have the chance to sector discomfort into remainder versus activity parts and dressmaker treatment to mobilization goals. Programs straightened to PUAEME008 offer discomfort management often consist of brief drills with standardized clients: take a 60 second discomfort history, state your functioning diagnosis out loud, call your first line treatment, and recognize two security concerns.
For physiotherapists, the assessment expands to work. If you measure the expense of pain in terms of minimized stride speed or failure to execute a sit to stand without breath holding, you can target analgesia to treatment home windows. Discomfort management training courses for physiotherapists ought to include just how to negotiate restricted pre therapy opioid dosing, the role of regional techniques like TENS or heat in multimodal plans, and just how to record action in practical terms that assist medical colleagues.
Choosing analgesia well: multimodal by default
Multimodal analgesia is not a trend, it is a protective concept. No single agent should lug the entire concern, which decreases the dose and negative effects of each component. Also in emergency situation settings, time allows easy mixes: acetaminophen within its daily restriction, an NSAID if kidney and bleeding threat permit, courses in pain management for nurses a small titrated dose of an opioid for severe discomfort, plus non pharmacologic actions like altitude or immobilization. In sickle cell discomfort, individual managed analgesia and hydration procedures surpass sporadic boluses and create fewer confrontations.
A recurring issue in practice is jumping to high opioid doses when a local or regional technique would do more with much less threat. A lower arm crack splints better after a hematoma block. Rib fractures might respond to a serratus former plane block, boosting ventilation and decreasing systemic opioid demand. Discomfort monitoring training programs need to educate clinicians to believe regionally and know their limitations, after that to involve acute pain or anesthetic colleagues when a block will alter the course.
For nurses who take most calls after hours, understanding short, defensible methods helps. A pain monitoring certification training course can provide basic decision tools: if discomfort at rest persists above a defined threshold after two hours of arranged non opioid therapy and the patient has no red flags for instability, you may administer a small rescue dosage per standing order, after that reassess and notify. These frameworks avoid both undertreatment and unstructured escalation.
Monitoring with function, not sketchy tick boxes
Monitoring is where safety often breaks. We examine sedation scores and breathing prices, after that stop working to act on fads. A program that rehearses pattern recognition adjustments that. If the client's breathing rate is drifting from 18 to 12 over 15 minutes while snoring begins, you quit and reassess. Lower or hold the next dosage. Sit the client up, apply extra oxygen meticulously if required, take into consideration naloxone if hypoventilation proceeds, and record the chain of occasions and your rationale.
Equipment readiness belongs to surveillance. I have seen greater than one ward maintain naloxone secured a far-off cupboard. That is not a policy problem when a person is de saturating. Discomfort monitoring training for registered nurses ought to include a timed drill: locate oxygen, suction, bag shutoff mask, and turnaround agents, after that practice calling for aid plainly with SBAR. For prehospital medical professionals functioning to PUAEME008 offer pain management standards, the very same discipline applies inside a moving automobile where space is tight and back-up is mins away.
Documentation as scientific care
Good notes are not clerical chores, they are the memory of the group. When analgesia decisions fail, the lack of clear paperwork is often component of the story. Conversely, accurate, timely notes frequently stop duplication, overdose, and blame.

What requires to be recorded is not strange. The preliminary discomfort assessment including range option and useful impact, the functioning diagnosis, the precise representative, dose, route, and time, the client's verbal consent or, if implied, the context, and any type of negative impacts observed. Within 30 to 60 minutes, document action with a number and a story: "Discomfort from 8 to 4 at remainder, still 7 on activity. Moderate queasiness, no vomiting. Breathing rate 16, keeping discussion." If you differed a procedure, write why. If the patient declined an option, write that with their stated reasons. These information protect both person and clinician.
For groups, shared language issues. Settle on the discomfort ranges you utilize, the sedation scale for opioid tracking, and the thresholds that trigger activity. Pain administration training courses must include micro workouts where students revise vague notes right into exact entrances. It is remarkable how commonly "person worked out" conceals meaningful deterioration.
Ethics at the bedside: obligation, dignity, and fairness
Ethical pain treatment lives in grey areas. People ask for even more medicine when you worry about adverse effects. Families ask you to hold back when the individual demands alleviation. A regular flyer shows up with a background of lost scripts, in agony from an intense fracture. You suspect medication seeking and still owe take care of a genuine injury.
A strong discomfort administration accreditation balances beneficence and nonmaleficence with justice. Below are the principles I emphasize:
- Respect for the patient's account. Discomfort is subjective. You can confirm injuries, try to find disparities, and still deal with reported pain dignifiedly. Location structure around treatment rather than ethical judgment around the person. Proportionality. Some pain is serious and time minimal. Others are chronic with flares. Short acting opioids have an area in acute extreme discomfort, but they are not a default for persistent non cancer cells discomfort. Teach tapering, non opioid adjuvants, and sensible goal setting. Transparency and shared decisions. Talk simply regarding dangers. Welcome the individual to evaluate advantages and compromise with you. If you set limits for safety, state why and document that conversation. Equity. Implicit bias damages discomfort care. Studies have actually shown undertreatment among people of shade, ladies, and non English speakers. A training course ought to test students to audit their behaviors and remedy them with organized tools. Stewardship. Prescribers hold public trust fund. Avoid providing high threat combinations like benzodiazepines and opioids without clear signs and recorded surveillance. Refer to addiction medication early when appropriate.
These principles are not abstract. They form exactly how you react when a patient requests one particular opioid by brand, or when an associate tells you not to "feed the habit." Honest quality, sustained by policy, minimizes conflict and sustains much safer care.
The certain needs of emergency discomfort management
Emergency setups make complex every variable. Triage should identify time critical medical diagnoses while eliminating suffering. A patient with abdominal pain might need analgesia prior to imaging, which proof supports, yet clinicians still bother with masking indications. Pain monitoring training must give permission and care together: supply analgesia, keep reassessing, and record changes in examination findings.
There are patterns that are entitled to focus in emergency situation pain monitoring programs. In trauma, prevent repeated IM shots in unsteady individuals and support IV titration or local blocks when possible. In severe frustration, avoid opioids as first line for primary migraine headaches and focus on antidopaminergics, magnesium, and hydration. In renal colic, NSAIDs usually exceed opioids for convulsion control, however see kidney feature. In burns, very early intranasal fentanyl or ketamine can alter the whole resuscitation trajectory. Rehearsing these specifics brings the course beyond generalities.
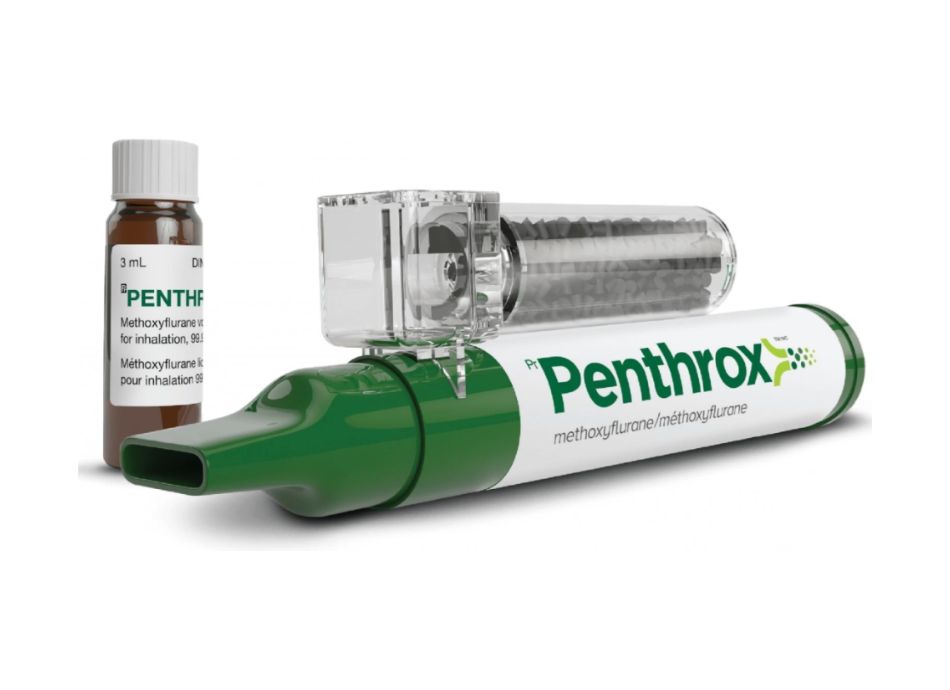
For paramedics straightened to structures similar to PUAEME008, the constraints are different: restricted formularies, variable IV gain access to, continual movement. Intranasal paths, breathed in methoxyflurane where permitted, and dental agents have outsized functions. Security hinges on careful individual option, clear contraindications, and durable handover to receiving groups with times, dosages, and actions recorded.
Building proficiency with circumstances and debriefs
The best supply pain administration course I ever ran used a rotating rhythm: a short targeted talk, a circumstance that placed that teaching to function, after that a debrief that drew the discovering into practices. In one situation, a person with rib cracks and light COPD called for repeated rearranging for x rays. The group that bore in mind to pre medicate prior to movement, trained breathing, and used a tiny dosage of ketamine for procedural resistance saw oxygen saturation enhance rather than decline. They also recorded each treatment and reaction, which aided the confessing group proceed the plan.
Debriefs ought to concentrate on thought procedures as high as actions. Why did you pick that agent? What were you expecting? Which indicator would certainly have made you quit and transform tack? This metacognition constructs the judgment genuine practice needs when you do not have time to ask a colleague.
Special populaces and edge cases
Learning increases when we check out the sides. A solid discomfort monitoring training course addresses groups where standard methods often break.
Children. Age suitable dosing and courses issue. Intranasal fentanyl can be a quick, non intrusive bridge. Weight based acetaminophen and ibuprofen schedules need to be specific. Habits cues supplement discomfort scales. Parents are companions, and their mentoring can decrease distress.
Pregnancy. Avoid NSAIDs in the 3rd trimester because of ductus arteriosus risks and kidney results. Acetaminophen remains initial line. Regional methods and non pharmacologic measures play bigger roles. Opioids can be utilized meticulously for serious discomfort with obstetric input.
Renal and hepatic impairment. Dosage changes and representative choice are not optional details. For instance, morphine metabolites build up in kidney failure and increase sedation danger. Hydromorphone might be more secure at low doses. Acetaminophen is secure at decreased optimum day-to-day dosages in secure liver illness, however warn powers throughout severe injury.
Opioid resistance and use condition. Higher opioid dosages may be required for analgesia, but the strategy should include surveillance and, ideally, dependency medicine involvement. Buprenorphine can be continued and supplemented for acute pain with professional input. Documentation is important to browse risk and offer sensible care.
End of life care. The moral goal shifts from treatment to comfort. Symmetrical opioid dosing, adjuvants for neuropathic elements, and courses that reduce problem, such as subcutaneous mixtures, must be taught. Family members require clear explanations to minimize concern of quickening death.
What a durable curriculum covers
Designing discomfort monitoring training for registered nurses or a certificate course hurting administration for blended clinicians implies mapping expertises to exercise truths. The core components normally consist of:
- Foundations. Pain physiology, types of discomfort, evaluation devices, and feature concentrated goals. Pharmacology. Dosing varieties, adjustments, interactions, and adverse impacts for common analgesics, consisting of acetaminophen, NSAIDs, opioids, ketamine, gabapentinoids, and topical agents. Techniques. Safe titration, client regulated analgesia essentials, breathed in agents where suitable, and an introduction to regional anesthetic with recommendation pathways. Safety and surveillance. Sedation scoring, breathing surveillance, prep work for degeneration, and reversal agents. Documentation and communication. Structured note writing, handover structures, lawful factors to consider, and consent. Ethics and equity. Prejudice recognition, stewardship, shared choice making, and pain care in substance usage disorders.
For organizations that provide a pain administration certificate, functional assessment matters. Simulation with straight observation, graph audits, and situation write ups generate more reliable capability than numerous option examinations alone. When the certificate signals that a clinician can safely deliver analgesia, instructors owe the general public that rigor.
How registered nurses, physio therapists, and doctors discover together
Multidisciplinary training increases the quality of care. Pain monitoring courses for nurses and discomfort administration training courses for physiotherapists take advantage of shared circumstances that force settlement. The nurse who knows the physiotherapist will certainly set in motion a knee arthroplasty person after lunch will certainly time a development dosage or suggest a local bolus prior to therapy, not after. The physio therapist that understands sedation risks will change the session as opposed to pressing with drowsiness.
Doctors usually lead prescribing yet rely on registered nurses for monitoring and feedback. Programs that include function switched simulations teach each self-control what the other sees. I have actually enjoyed a junior medical professional role play an evening nurse handling three mixtures and come away much more mindful with PRN orders and more clear with hold parameters.
Legal frameworks and regional policy
Courses ought to anchor technique in regional law. PUAEME008 Supply Pain Management in the Australian employment structure lays out expertises for prehospital treatment, consisting of secure selection and management of analgesia and surveillance. Health center credentialing policies specify who may launch certain agents or techniques. National standards frequently advise multimodal analgesia and opioid stewardship principles like using the lowest efficient dosage for the quickest needed duration. Pain management accreditation courses that ignore these rules generate friction and risk.
Learners need absorbable summaries of what uses in their solution. Include standing orders, escalation pathways, and documents themes that satisfy lawful assumptions. Where a legal criterion is vague, adopt a conventional, defensible neighborhood procedure and educate it consistently.
Measuring end results and improving the course
If you run an offer pain monitoring course, audit results. Track rates of undertreated discomfort at discharge, naloxone administration after inpatient analgesia, time to first analgesic in triage, and paperwork completeness. Numbers do not tell the whole tale, however they expose patterns. A ward that consistently postpones analgesia after hours may need standing orders and registered nurse launched methods. A spike in over sedation may point to dosage errors or voids in keeping an eye on skills.

Feedback from learners matters as well. Ask what components felt straight valuable on the next change. Modify instances to mirror real local obstacles, such as minimal access to regional anesthesia after hours or regular transfers between centers with different formularies. A discomfort management certification must advance with method and policy.
The value of brief training courses versus deeper certification
Short training courses suffering management have a place. A focused half day on emergency analgesia can hone triage methods and decrease time to alleviation. A component for physiotherapists on pre therapy application and documents can streamline entire wards. Yet some roles demand deeper training. A discomfort monitoring accreditation training course that extends several weeks, includes mentored medical method, and culminates in evaluation generates leaders that can show others and steward protocols.
When supervisors ask which to fund, I suggest a layered strategy. Offer a wide someday training course to many medical professionals, then sponsor a smaller cohort for the certification course suffering management who will serve as regional champs. Set education with plan, audit, and comments loops to sustain change.
Final ideas from the field
Patients remember whether we took their discomfort seriously and whether they felt risk-free. Medical certificate course in pain management professionals remember the situations that failed and the paperwork that safeguarded a great telephone call made under stress. A well built offer pain management course weaves safety, documents, and values right into every professional choice, from the initial dose at triage to the last note prior to handover.
For those seeking a discomfort administration certificate or designing pain administration training courses, aim for realistic look. Show the pharmacology specifically, then stress test it with side cases. Insist on documentation that might stand alone if you went off change mid dilemma. Call the honest stress and practice the words to navigate them with patients and colleagues. That is exactly how training turns into far better treatment on the ward, the road, and the clinic.
Below is a portable list that numerous teams locate useful at the bedside. It does not change judgment, however it triggers the ideal relocations at the ideal time.
- Assess: type of pain, seriousness at rest and on motion, red flags, function. Plan: multimodal approach, dosage and course customized to comorbidities, keeping track of plan. Prepare: turnaround representatives offered, oxygen and suction available, acceleration pathway clear. Act: carry out, coach non pharmacologic actions, reassess within defined windows. Document: analysis, reasoning, doses, responses, adverse impacts, shared decisions.
Whether you operate in a jampacked ED, a rural ambulance, or a recovery health club, the craft of pain care coincides. Start with respect for the patient's experience, use the tools carefully, and leave a clear route for the following medical professional. If a discomfort management accreditation helps you construct those routines, it is worth every hour invested.